What is Low Vision?
“Low vision” is the impaired vision that cannot be fully restored by surgery, medical treatments, or conventional eyeglasses or contact lenses. Low vision is not blindness. You are not alone; over 15 million Americans have some form of visual impairment. We are here to help. You can do something about low vision.
Our goal is to help you make the most of the eyesight you have so you can do more of the things you need and want to do — whether it’s reading a book, writing a letter, shopping, watching television or doing crafts.
When an individual’s eyesight cannot be corrected to better than 20/200 with lenses, then he/she is diagnosed as having low vision. Macular degeneration, diabetic retinopathy, and genetic diseases are just some of the causes of this diminished vision.
Unfortunately, many people are told that nothing can be done. While there may not be a cure, we can design and prescribe low vision systems for many of these individuals. Bioptic telescopes and microscopes are mounted in a pair of glasses to allow many of them to resume reading, cooking, hobbies, playing cards and in some cases driving – greatly improving their lifestyles.
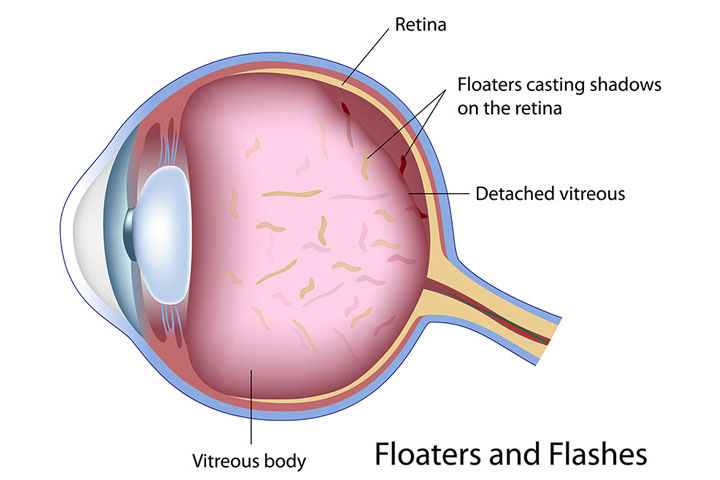
Floaters & Flashes
As we get older we expect to have problems with our eyes, so we tend to ignore them.
One minor symptom that can cause a bigger problem, if not treated, is the occurrence of floaters and flashes. These are those tiny lights that seem to blink through your vision and that you can never catch when you direct your focus toward them.
Almost everyone sees floaters at some time, but they can occur more frequently and become more noticeable as we get older.
In most cases, no serious problems are found, but a complete eye examination is important. If there is damage to the retina, it needs to be diagnosed and treated immediately to prevent vision loss.
Conjunctivitis
Conjunctivitis, sometimes referred to as pink eye, is an infection or inflammation of the conjunctiva – the thin, protective membrane that covers the surface of the eyeball and inner surface of the eyelids. It can be caused by bacteria, viruses and other germs that are transmitted to the eye through contaminated hands, towels, and eye makeup or extended wear contacts. It can also result from exposure to irritants such as chemicals, smoke or dust; or by pollen and other allergens. It is not uncommon for conjunctivitis to accompany a cold or flu.
Bacterial or viral conjunctivitis is contagious and tends to be prevalent in daycare centers and schools. It can spread by direct person-to-person contact, in airborne droplets that are coughed or sneezed, or from sharing makeup, towels and washcloths. Its hallmark sign is redness in the white of the eye that may be accompanied by increased tearing and/or a discharge that is watery or thick with mucus and pus and causes the eyelids to stick together.
Although usually a minor problem that improves within two weeks, some types can develop into serious corneal inflammation and vision loss if not treated. If you wear contact lenses and suspect you have conjunctivitis, discontinue wearing your contacts until the condition clears; you may also need to replace your contact lenses to prevent a recurrence.
There are four primary types:
Bacterial conjunctivitis can affect one or both eyes and is usually accompanied by a heavy, yellow discharge that may cause the eyelids to stick together in the morning. Caused by a variety of bacteria, bacterial conjunctivitis is treated with antibiotic eye drops and typically resolves within 5 days. If there is concurrent inflammation of the eyelids, your eye care provider may also recommend an eyelid scrub to remove bacteria and dried mucous from the lid margin.
Viral conjunctivitis is often caused by adenoviruses, the family responsible for upper-respiratory illnesses such as colds, but can also result from herpes simplex and other viruses. This type can also affect either one or both eyes, and usually causes a lighter discharge. Although viral conjunctivitis usually produces a superficial case that clears on its own within two weeks, you should still see your eye care provider to ensure it doesn’t lead to a more serious infection that can involve the cornea.
Antibiotics are ineffective for viral conjunctivitis. Artificial tears may be used, or your doctor may recommend a topical anti-inflammatory drop to relieve discomfort. Topical or oral anti-herpetic medications can help suppress herpes viral infections.
Allergic conjunctivitis results from a response to airborne pollen, dust, smoke, or environmental agents. Both eyes are usually affected and may itch, tear excessively and discharge a stringy mucus. You may also have other allergic reactions, such as a runny or itchy nose. Depending on the severity, your eye doctor may prescribe topical drops that are effective in relieving the itching and discomfort. A very specific kind of allergic conjunctivitis may occur in contact lens wearers, especially if they do not clean the lenses well or if the lenses are not replaced often enough. Several treatments are available for this condition, including prescription allergy drops, changing contact lens solutions to keep the lenses cleaner, and changing to lenses that are replaced more frequently such as daily disposable contacts.
Chemical conjunctivitis is caused by exposure to irritating liquids, powders, or fumes and requires immediate action. Common irritants in include chlorine, detergents, fuels, ammonia, smoke and pesticides. First, flush the eye with cold water continuously for 15 minutes, then have the eyes evaluated by your eye doctor. For minor irritants such as chlorine, often artificial tears will effectively resolve the irritation. For chemicals burns from a strong acid or base, emergency medical treatment is needed.
Conjunctivitis- Signs and Symptoms
Viral conjunctivitis
- Watery Discharge
- Irritation
- Red Eye
- Usually begins with one eye but may spread easily to the fellow eye
Allergic conjunctivitis
- Usually affects both eyes
- Itching
- Tearing
- Swollen eyelids
Bacterial conjunctivitis
- Stringy discharge that may cause the lids to stick together, especially after sleeping
- Swelling of the conjunctiva
- Redness
- Usually affects only one eye but may spread to the fellow eye
If you suspect conjunctivitis, see an eye doctor as soon as possible.
Your eye will be examined to determine the specific cause of the inflammation and your eye doctor will determine what the best course of treatment to resolve the condition.
People with conjunctivitis should:
- Wash their hands after touching or wiping their eyes
- Avoid touching other people unless hands are freshly washed
- Throw away or carefully wash items that touch their eyes
- Not share eye makeup or other items used on their eyes (for example, towels, or tissues)
- Cover mouth and nose when coughing or sneezing
- Consult your doctor in case medication is needed
- See a doctor if the eye discharge is yellow, if the eye or eyelid is red, or if the symptoms don’t start improving after 2-3 days. See a doctor immediately if the symptoms suggest a more severe infection
- Be excluded from school and child care settings until cleared by a health care provider that it is not contagious, after taking antibiotics for 24 hours, or until symptoms have resolved
Ocular Allergies
Allergies affect over 20% of the general population and are on the rise in many developed countries. The specific reason for the increasing prevalence of allergies has not been determined; some believe it is due to the effects of pollution in urban areas while others consider that modern lifestyles don’t allow for enough childhood exposure to allergens to become acclimated to them.
Allergies can take many forms, affecting various organs or tissues. Ocular allergies are among the most bothersome forms of allergic reaction.
The Eyes’ Response to Ocular Allergens
When exposed to these allergens, the response in the eye is nearly immediate:
- First, itching sets in and can become persistent and extremely bothersome if exposure to the allergen is continued.
- Sortly after itching, redness of the eyes follows and can last somewhat longer, as the blood vessels of the eye are slower to recover.
- The swelling of the eyes and eyelids comes to its peak later than the itching, as swelling is also caused by the blood vessels letting fluids out into the tissue around them. Swelling is the sign of ocular allergies slowest to disappear, due to the time it takes for the displaced fluid to be removed.
- The itching can be considered the most uncomfortable symptom, whereas the swelling and redness are most bothersome in terms of appearance.